Sepsis, commonly known as blood poisoning, is usually caused by the infections of bacterial which enter the patient’s bloodstream through open wounds and even urinary tract infections. There are 15700 new cases of sepsis in Australia every year, of which more than 5000 people die, and some survivors are amputated or even permanent disability. The cost of treatment for each sepsis patient treated in the intensive care unit (ICU) is close to $40,000 AUD.
According to a new survey in Australia, only 40% of people have heard of sepsis, let alone specific symptoms of sepsis. Nowadays, more and more people are beginning to realize the globalization of sepsis. If more people understand sepsis, we may be able to detect and even intervene as soon as possible, which may improve the survival rate of many patients. World Health Organization (WHO) has called on the global community to scale-up global advocacy, funding, and research capacity for epidemiological evidence of sepsis; develop rapid, affordable, and appropriate diagnostic tools, especially at the primary and secondary health levels, to improve the diagnosis, monitoring, prevention and treatment of sepsis.
Two stages of sepsis
The first stage occurs when the infection enters the bloodstream, and the body’s immune system overreacts, commonly known as hyperinflammatory immune response, which can lead to multiple organ failure. This stage usually lasts 7-10 days or more, depending on the severity of the infection. If the patient is not treated successfully and effectively in the first stage, he or she will then enter the stage of immune paralysis. At this stage, the patient’s immune system can no longer resist infection, and patients may have nausea and vomiting, red spots on the skin, reduced urine output, shock, and even death.
Sepsis can affect anyone, and it is especially dangerous for the elderly, pregnant women, children under one-year-old, and people with weak immune systems (premature babies or people with chronic diseases). Patients in the ICU are prone to infection, which can also lead to sepsis.
Symptoms of sepsis
There are many pathogens that cause sepsis, but bacteria account for almost 80%, while pathogenic fungi and viruses account for the rest proportion. Based on this, patients with sepsis have different symptoms and usually have superinfection. If the patient has symptoms of infection and is accompanied by low systolic blood pressure, high fever, and increased respiratory rate, he or she is diagnosed with sepsis.
Diagnosis of sepsis
The current methods for screening patients with potential sepsis are systemic inflammatory response syndrome (SIRS) criteria, heartbeat and respiratory rate, body temperature (min/max), and white blood cell (WBC) count. Hospitals and ICU implement sepsis treatment programs based on these standards at slightly different times. Positive cases trigger the first step in determining the source of infection. Recognizing a bacterial infection requires up to 5 days of culture to get a negative result, which is longer than the progression of the disease itself. This non-specific tool, coupled with the heterogeneous early symptoms inherent in sepsis, is the main reason for the difficulty in identifying, diagnosing, and managing this deadly disease. Thus, there is an urgent in developing a rapid, affordable, and appropriate diagnostic tool.
Studies have shown that cell surface and proteomic markers are viable biomarkers for sepsis. Engineering point-of-care (POC) platforms may be important for quantifying various biomarkers (as fingerprints of the immune system for early sepsis). They allow patients to test these biomarkers before coming to emergency rooms and hospitals, or to test these markers quickly in the hospital for rapid stratification of the patient and the disease. Different stages of sepsis have different biological characteristics, leading to different treatment requirements, which can be diagnosed by providing rapid and accurate biomarker information.
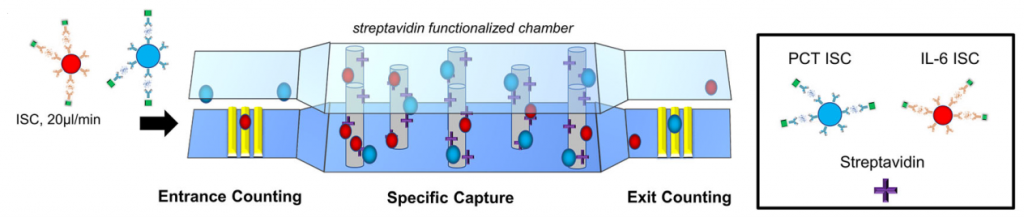
Therefore, Professor Bashir (Dean, Grainger College of Engineering, University of Illinois at Urbana-Champaign) and his colleagues established a microbead detection platform for the simultaneous detection of PCT and IL-6 (abnormal PCT and IL-6 levels can be used as diagnostic and prognostic markers for sepsis, respectively), and it was tested on spiked undiluted human plasma samples (Figure 1). They first established PCT (LOD 130 pg/mL) and IL-6 (150 pg/mL) microbead sandwich immunoassays, respectively, and verified their compatibility with multiplexed capture using flow cytometry. Two commercially available carboxyl active magnetic microbead populations (Absolute Mag™ Carboxyl Magnetic Particles, WHM-S035, WHM-S034, CD Bioparticles) with mean diameters 9 μm and 7 μm were coupled with carbodiimide crosslinker chemistry to the primary PCT and IL-6 capture antibody respectively. These immune sandwich complexes (ISC) simultaneously capture different ranges of PCT and IL-6 from a single undiluted plasma sample and flow through the established microfluidic biochip platform. Professor Bashir said, “This new application demonstrated the ability to differentiate with significance, varying expression conditions for both PCT and IL-6 in the clinically relevant range of potentially septic patients. Several improvements are necessary for both increases in quantification range and clinical application.” However, as proof of principle, this manuscript emphasizes this multi-channel capture detection platform promising to distinguish healthy and potential sepsis patients with different PCT and IL-6 concentration ranges. Detailed results are published on Biomedical Microdevices.
Therapy for sepsis Patients is usually treated with antibiotics and dialysis because the kidney is one of the organs that are often affected when patients suffer from sepsis. Other treatments include blood purification to remove toxins, but there are few successful cases. Many doctors choose corticosteroid therapy, although this treatment can reduce patients’ time in ICU, the mortality rate does not seem to decrease, and more importantly, although corticosteroids can reduce inflammation in patients, it can also lead to a sharp decline in the number of immune cells in patients, which does not seem to be conducive to anti-infective treatment.
Reference:
Berger, J., Valera, E., Jankelow, A., Garcia, C., Akhand, M., Heredia, J., … & Tiao, J. (2020). Simultaneous electrical detection of IL-6 and PCT using a microfluidic biochip platform. Biomedical Microdevices, 22, 1-11.
